Switching regimens without relapse? Explore the truth of multiple myeloma patients with real-world study
2021-07-09 | Press Releases
Multiple myeloma (MM)
Multiple myeloma is a malignant disease characterized by an abnormal proliferation of clonal plasma cells and is the second most common hematologic malignancy in many countries. MM mostly occurs in elderly adults and is still incurable. It is difficult to objectively identify and evaluate market opportunities of MM via traditional research methods due to its complex lines of treatment, absence of effective drugs and long treatment cycle.
A variety of new mechanism and biotherapies are under development or have been marketed outside of China in this field, such as CAR-T, BCMA antibody-drug conjugate, etc., showing a great potential. In the near future, new products will also launch in China. The top priority for the successful launch of new products is to map the market strategies in advance and seek opportunities. We have done some exploration using real-world data in China.
1. The reason behind switching regimens without relapse
The Guidelines for the Diagnosis and Management of Multiple Myeloma in China (hereinafter referred to as the “Guidelines”) includes recommendations of frontline treatment, salvage treatment and primary drug resistance treatment for MM patients. In the standard treatment process, the timing of patients changing the treatment regimens is related to disease progression or non-remission of the disease, such as early relapse, late relapse and primary drug resistance. However, we have found through real-world study that approximately 50% of the patients still change their treatments despite having favorable efficacy assessment results, including MR, PR, VGPR, and CR. Besides, patients change regimens very frequently, with all newly diagnosed MM patients being treated with an average of 2.6 regimens before their first progressive disease (PD).
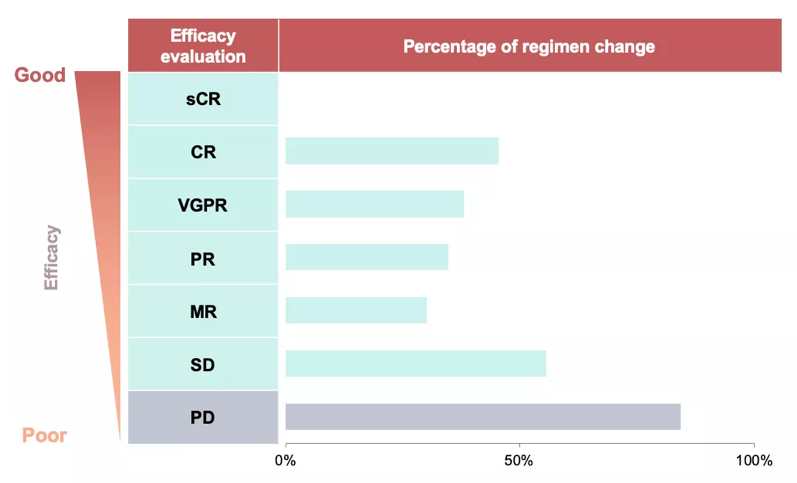
sCR-Stringent Complete Response; CR-Complete Response; VGPR-Very Good Partial Response; PR-Partial Response; MR-minimal response; SD-Stable Disease;
What causes half of the patients to switch regimens before disease progression? Through a more in-depth data mining and extensive interview with doctors, we find that about 5% of the patients with better efficacy assessment change regimens due to intolerable side effects while the remaining 45% change regimens pursuing for better efficacy.
Different HCPs have different treatment goals. Some HCPs’ definition for “good efficacy” is more stringent than others’. They believe that if patients can achieve deeper remission within shorter time period, better outcomes and prolonged overall survival can be obtianed. Therefore, these HCPs tend to add or switch drugs before patients’ disease progression.
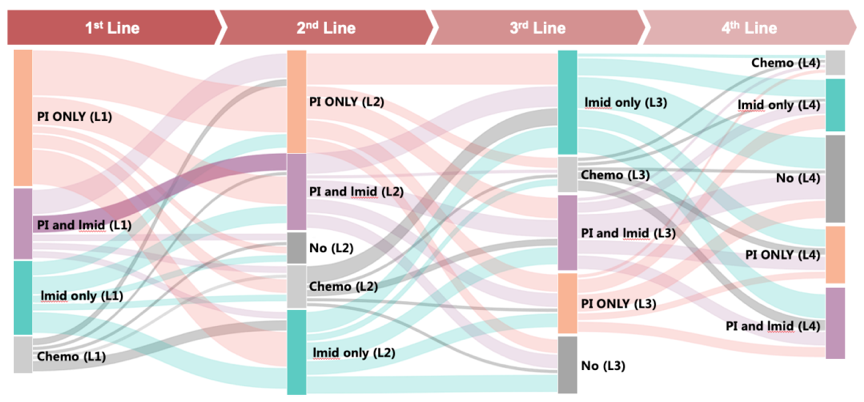
2. Real-world data insight – the switching of regimens
Which regimen, then, do patients in the progression-free group change from and which do they change to? At present, the main drugs used to treat MM in China include immunomodulators drugs (IMiDs, such as thalidomide and lenalidomide), proteasome inhibitors (PIs, such as bortezomib and ixazomib) and other chemotherapeutic drugs (such as dexamethasone, adriamycin, cyclophosphamide, etc.), of which the first two types are the core drugs for MM treatment. Patients’ treatment regimens switch between the treatment regimens composed of these three types of drugs, which can be summarized as below:
We further compare patients who change regimens after disease progression with patients who change without disease progression and find that the latter, with over 40% of them, nearly twice as many as the former, have added new mechanism drugs to their original regimen. Nearly 30% of patients with clear disease progression choose new mechanism drugs when changing regimens, a percentage more than twice the progression-free group.
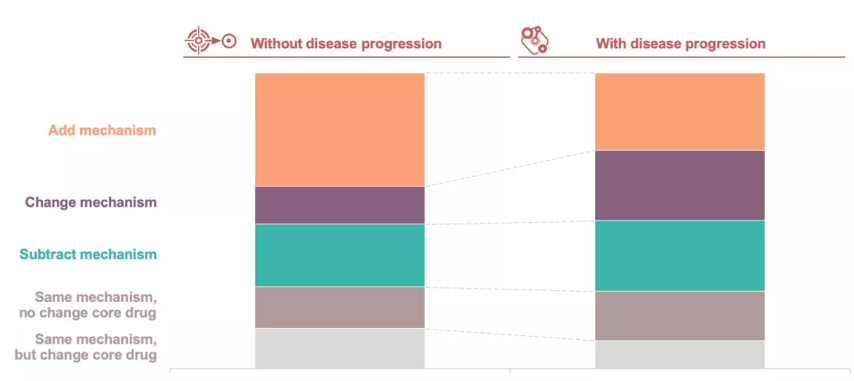
The analysis of the switching of regimens in two patient groups further confirms the views of HCPs in the interview: more patients without disease progression add new mechanism drugs to their treatment regimens for better efficacy, while patients with disease progression choose to change regimens or reuse the previous treatment regimens according to the relapse time and recommendations from the Guidelines.
These findings reveal the timing of MM patients changing regimens in the real-world setting - patients do not strictly follow the standard treatment pathway and only change their treatment regimens after relapse or drug resistance. Instead, they change their treatment regimens before disease relapse or refractory, and the proportion of these patients is up to 50%.
Through further analysis of the switching of regimens, we find that such patients are more likely to add new mechanism drugs when changing their treatment regimens, which coincide with some HCPs’ opinion of changing regimens for patients without disease progression for better efficacy.
Each regimen change brings a new decision node for treatment regimens, suggesting that for new medications coming in the field of MM, opportunities in the real-world setting often come earlier than perceived as indicated the guidelines. This is exactly the unique value of using real-world study to evaluate market opportunities, segment the market, and develop marketing strategies for innovative treatment regimens.
3. Conclusion
The study population in this case covers a wide range of geographic regions in China with high-granularity data throughout patients' whole process of diagnosis and treatment. The natural language processing technology of HLT facilitated the interpretation of unstructured medical texts and convert them into data models that can be processed by computers, so that statistical analysis of the diagnosis and treatment of patients can be done with authorization.
In this study, we quantitatively distinguishes lines of treatment for MM patients, outlines the market landscape of different lines of treatment, and specifies the target population of the product. We are also building sales prediction models to estimate resource investment for the product.
Real-world data covers a variety of dimensions, thus can reproduce the situation of the market in a complete manner, and provide a comprehensive understanding of the market. With authorization on analyzing real-world data, it is easier to touch upon the "blind area" and identify the information that cannot be covered by traditional market research. More valuable market insights can be obtained by combining these results with the ones from traditional market research. The market insights can not only identify new opportunities, but also help healthcare professionals understand the unmet needs, improve the diagnosis and treatment, and benefit the patients.
In addition, highly efficient data processing techniques such as machine learning, real-time iterative analysis and other advanced analytical appraoches provide better methodological support for real-world studies. For more information about the potential of real-world research, please contact us.
Reference
The Guidelines for the Diagnosis and Management of Multiple Myeloma in China. Chinese Journal of Internal Medicine, 2017, 56 (11): 866-870.


 津公网安备 12011502000526号
津公网安备 12011502000526号